This study [1] arose out of a clinical aspiration to do things better. Daily practice in secondary care spinal clinics at a large metropolitan hospital saw distressed and disabled patients with low back pain (LBP) come and go. Many had waited months or years for ‘surgical’ consultation, only to be promptly discharged – with “community-based conservative management” the mainstay of advice on offer.
In this government-funded setting with limited resources it was enticing to consider that early patient screening to identify those most at risk of a poor outcome, could offer potential for the timely delivery of care to those most in need. This made intuitive sense as an approach likely to both optimise patient outcomes and have cost benefits. For this approach to work, however, screening needed to be able to provide accurate prognostic information.
It was here we hit a stumbling block. Most screening approaches for low back pain have been developed [2-4] and implemented [5, 6] in primary care settings. Positive outcomes from targeted management strategies have been reported, yet recent evidence suggests a need to question the prognostic accuracy of popular screening instruments [7]. Since misclassification of patient risk was common in primary care settings (using tools designed for primary care) – skepticism about their value in secondary care settings was warranted.
To investigate this we recruited 220 patients who had been referred to the spinal outpatient service and placed on booking queues. Participants completed baseline outcome measures and 3 screening instruments, and were followed up 4 months later (while still on the booking queue). We performed a head-to-head comparison of the 3 instruments: the Keele STarT Back Tool (SBT)[3], the short-form Orebro Musculoskeletal Pain Screening Questionnaire (OMPSQ)[8] and the Predicting the Inception of Chronic Pain Tool (PICKUP)[2]. Specifically, we examined their ability to discriminate between participants who would and would not have a poor outcome 4 months later. We defined ‘poor outcome’ as a score of 3 or above on 11-point rating scales for pain intensity and/or disability. (We chose this dual classification because we considered that participants with scores of <3 for pain and <3 for disability are likely to consider themselves to be recovered. Scores of >3 on either scale would indicate a poor outcome.) We also applied a novel statistical approach that compared (hypothetically) the value of screening patients to guide management decisions with an approach offering treatment to all patients.
While we knew that patients referred to spinal outpatient clinics were often already on a problematic road, we were still surprised to find that 84% of the 195 participants met our criteria for poor outcome at follow-up. We found that the instruments classified a patient’s individual risk of a poor outcome with an accuracy of between 60% and 70%; mostly underestimating risk. When we (statistically) weighed the probability of the screening instruments misclassifying patient risk against the benefits of screening (i.e. correct allocation of care) we found that the screening strategies offered no overall advantage over a strategy of providing care to all patients. Instead, our findings suggested that care decisions in this setting should be made with the assumption that all patients are at risk of an unsatisfactory recovery.
At the outset, we had in mind a next step: to undertake a randomized clinical trial to evaluate the benefits of implementing care pathways targeted according to ‘risk’ – informed by a ‘useful’ instrument. Our study indicates however, that to progress in this manner is probably not warranted in this cohort. Using these instruments (developed for primary care), to direct treatment decisions in secondary care, is at best not helpful and probably unhelpful. Modified screening strategies with the potential to offer clinical value in secondary care settings need to be further considered.
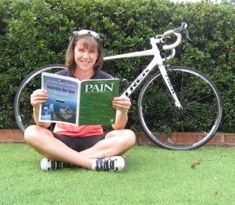
About Emma Karran
 Emma Karran has a background in clinical Physiotherapy and education. She is a current PhD candidate with the Body in Mind Research Group at the University of South Australia, supervised by Prof. Lorimer Moseley. She is supported by grant and scholarship funding from the Royal Adelaide Hospital Research Foundation.
Emma Karran has a background in clinical Physiotherapy and education. She is a current PhD candidate with the Body in Mind Research Group at the University of South Australia, supervised by Prof. Lorimer Moseley. She is supported by grant and scholarship funding from the Royal Adelaide Hospital Research Foundation.
References
[1] Karran EL, Traeger AC, McAuley JH, Hillier SL, Yau Y-H, Moseley GL: The value of prognostic screening for patients with low back pain in secondary care. The Journal of Pain 2017.
[2] Traeger AC, Henschke N, Hübscher M, Williams CM, Kamper SJ, Maher CG, Moseley GL, McAuley JH: Estimating the Risk of Chronic Pain: Development and Validation of a Prognostic Model (PICKUP) for Patients with Acute Low Back Pain. PLoS Med 2016, 13(5):e1002019.
[3] Hill JC, Dunn KM, Lewis M, Mullis R, Main CJ, Foster NE: A primary care back pain screening tool: identifying patient subgroups for initial treatment. Arthritis Rheum 2008, 59.
[4] Shaw WS, Pransky G, Winters T: The Back Disability Risk Questionnaire for work-related, acute back pain: prediction of unresolved problems at 3-month follow-up. J Occup Environ Med 2009, 51(2):185-194.
[5] Hill JC, Whitehurst D, Lewis M, Bryan S, Dunn KM, Foster NE, Konstantinou K, Main CJ, Mason EE, Somerville S et al: Comparison of stratified primary care management for low back pain with current best practice (STarT Back): a randomised controlled trial. The Lancet 2011, 378:1560-1571.
[6] Foster NE, Mullis R, Hill JC, Lewis M, Whitehurst DG, Doyle C: Effect of stratified care for low back pain in family practice (IMPaCT Back): a prospective population-based sequential comparison. Ann Fam Med 2014, 12.
[7] Karran EL, McAuley JH, Traeger AC, Hillier SL, Grabherr L, Russek LN, Moseley GL: Can screening instruments accurately determine poor outcome risk in adults with recent onset low back pain? A systematic review and meta-analysis. BMC Medicine 2017, 15(1):13.
[8] Linton SJ, Nicholas M, MacDonald S: Development of a short form of the Orebro Musculoskeletal Pain Screening Questionnaire. Spine 2011, 36(22):1891-1895.
Commissioning Editors Carolyn Berryman and Mark Catley