Five early-career pain researchers are participating in the PRF-NAPS Correspondents program during the 2024 North American Pain School, taking place 23-28 June in Montebello, Québec City, Canada. The Correspondents program is a unique science communication training program that provides participants with knowledge and skills needed to communicate science effectively to a wide range of pain researchers, patients, and the greater public. The Correspondents will conduct interviews with NAPS Visiting Faculty and Patient Partners and provide live blogging, too! Take a look at their blog posts below.
NAPS Day 1 Blog Posts
Careers Don’t Have to Be Linear
How the West Has Won (over the Crowd, Not the Stanley Cup)
Careers Don’t Have to Be Linear
The sun is at my back, the wind is gently blowing over the water, and the view is magnificent. As I write this blog, I’m taking a moment to enjoy the present, realize the privilege of being seated here, and absorb our first day at NAPS.

I feel like my brain is full with new information about pain. Several exceptional presentations and conversations have made me realize how fascinating, yet complex, the world of pain is.
“Careers don’t have to be linear. They can have many wonderful twists and turns.”
This sentence from Jessica Merlin (University of Pittsburgh School of Medicine, Pennsylvania, USA) moved me yesterday.
With the end of my PhD approaching, questions about my next steps can no longer be avoided and are causing significant stress.
Do I need a postdoc? Should I go abroad? Pursue a clinical doctorate? Leave academia and find my own path? What awaits me?

Image courtesy of Shutterstock
I feel this insecurity associated with the end of the doctoral journey is not unusual, but it’s often something no one dares to talk about. We secretly hope to get a professor position and continue doing research without realizing that this dream can be difficult to achieve. I’m a statistics girl, and stats don’t lie about engagement rates. The fact that less than 20% will achieve a professorship is scary.
What’s great about NAPS is that we dare to talk about it. By sharing her atypical journey, Jessica allowed me to question my future without feeling the pressure of perfection. Calia A. Torres (University of Alabama, USA) also addressed the ups and downs in the race for a professor position, and her authenticity was so refreshing.
After our first day at NAPS, I haven’t solved the mystery of my future, but I’ve been able to reconcile my wish for the “perfect path.”
As Melanie Noel (University of Calgary, Alberta, Canada) said, the most important thing is to “choose life.” A life that will make you happy.
Marimée Godbout-Parent is a PhD candidate at the Université du Québec en Abitibi-Témiscamingue, Canada. You can follow her on Twitter/X – @marimeeparent12.
How the West Has Won (over the Crowd, Not the Stanley Cup)
Today’s “self-actualization journey” update: 30% complete.
Although it’s technically the “first full day of NAPS,” it already feels like I’ve known these people for years. The endless talks with my peers and intriguing concepts discussed by mentors have given me such validation, excitement, and hope for the future!
Some evidence is as follows:
- Jennifer Haythornthwaite (Johns Hopkins University, Maryland, USA) at Sunday dinner spoke about the wisdom of an academic route, and how it takes bravery and self-reflection to advocate for our passions to build a better life.
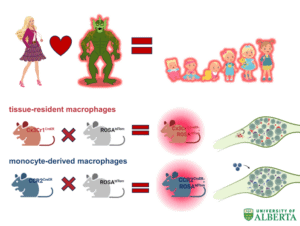
- Sharing my research to the crowd and winning over so many with my silly analogy about sea monsters and macrophages.
- At Monday lunch, I chanced upon a few peers who were my niche interest group and put a face to the researchers’ names adjacent to the papers I’ve admired – which knocked down barriers I never knew I placed upon myself.
- Calia A. Torres shared her realistic and humanizing career journey, and how too much structure can sometimes impede a richly lived experience.
- Despite Monday night’s brutal loss by the Oilers hockey team, pushing authenticity as an Edmontonian among non-Albertans allowed me to stand out with a unique icebreaker, which is often challenging when trying to make an impression towards potential collaborators or mentors.
All that in less than 48 hours, and so much more you probably don’t want me to get into. In these two days, I have observed a community already being forged and dedicated to resolving pain. If you want results™ from research, you start with the researchers themselves. If there were a place to look for the fabled “magic bullet” that cured pain (at the risk of sounding cheesy), it would be at NAPS. I honestly can’t wait for the next few days. How can you top this feeling?
Madelene Faye Ho is a PhD student at the University of Alberta, Canada. You can follow her on Twitter/X and Instagram – @iammadho.
The first official day at NAPS has come to a close, and what an amazing day indeed! As if kick-starting the day with delicious smoothies and a yoga session led by the wonderful Ondine wasn’t enough, our day was jam-packed. We listened to trainee presentations, Visiting Faculty lectures, and had our first interactive NAPS workshop.
Jessica Merlin shared her pearls of wisdom for navigating the world of grad school, academia, and establishing yourself as an independent researcher. She did a fantastic job normalizing this journey and explained it’s not linear or earned. A quote that stuck out to me during her lecture was, “Run screaming towards the fire.” She used this (rather visual) quote to contextualize our research of understudied populations who need the most help.
A lot of our trainee presentations took place today, which is something I always look forward to at conferences. I was blown away (and humbled!) by the amount of incredible work that is being done by trainees at different points in their educational journeys. While we all focus on different aspects of pain, we are unified in our mission to serve.
Our last session of the day was led by the enthusiastic Jennifer Haythornthwaite. She led an interactive workshop about making the most of your mentors. It was helpful to work through “tricky” scenarios and learn how fellow NAPSters and faculty would cope. I also enjoyed her overview of the reciprocity that is embedded in a true mentor-mentee professional relationship.
Our day came to a close in the best way – sitting around a bonfire, bathed in bug spray, listening to guitar, and stuffing our faces with s’mores. If every day was like this one, I wouldn’t be upset.
Morgan MacNeil, RN, is a PhD candidate at Dalhousie University, Canada. You can follow her on Twitter/X – @morganxmacneil.
Writing this Monday evening, I find it difficult to believe it’s only been a day-and-a-half at NAPS! I’ve heard this sentiment echoed by others, too. Every minute has been filled with opportunities, and each brief conversation feels impactful.
The NAPSters group is just the right size – we’re small enough that faces are becoming familiar, but there are still plenty of people I have to meet. Talks given by the Executive Committee and Visiting Faculty have been very inspirational. These range from learning about Calia A. Torres adapting to life’s challenges, seeing Gregory Corder’s “Dune Pain Box” go from sketches in 2014 to fully developed in 2019 (University of Pennsylvania, USA), and hearing Jessica Merlin’s passion for helping those with complex HIV chronic pain conditions.
The student presentations have also been brilliant. The five-minute presentation format has helped me absorb new information from different fields without getting overwhelmed. It also acts as a great conversation starter to approach others after their talk and bounce ideas between fields.
One stark difference that came up between the basic and clinical fields is how human studies are keen to investigate individual variability, whereas basic research tries to control variability as much as possible. There were many “Aha!” moments as the clinical researchers learned that gene therapy is only done in mice and not rats, and the basic researchers learned about the care that must be taken with conclusions in human studies that may affect policy decisions.
Despite this being a “North American” pain school, many of the trainees originally come from around the world, so the diversity in perspectives has been refreshing. Like the fireflies I got to see on the first night at NAPS, I’m awed by the sparks flying everywhere among us trainees.
Rima El-Sayed is a PhD candidate at the University of Toronto, Canada. You can follow her on Twitter/X – @RimaElSayed1.
The first day of NAPS is in the books, and I can’t remember half of what we learned about. If the specifics elude me, however, I can still see a general theme: If there is a broad, effective treatment for chronic pain – a “magic pill” – can we find it? If we found it, can we implement it?
What would it take to find a magic pill for pain? Intimate collaboration among patients, clinicians, and researchers to identify patient needs, integrate those with clinical findings, direct basic research towards promising topics, and bring the results of that research back to the clinic.
Clinicians would need real time with patients to deeply understand the biological, psychological, and social contributors to their pain. The system would need to be agile so researchers could pivot to study promising leads, and efficient in moving these findings through the translational-to-clinical pipeline and into accepted practice. Does that sound like the world we live in?
Let’s say we do find the magic pill for pain. Would it be adopted into clinical practice overnight? Even the most effective treatment would face barriers to implementation. Providers would need time to educate their patients on (yet another) new intervention. Patients would need to be able to access this new intervention. More than once today, the conversation around pain treatment became one of access. Pain patients may lack insurance, preventing them from accessing any care. Insurance companies may deny new treatments until the patient has failed more “conventional” approaches. Wait lists for pain clinics are months to years long.
The magic pill may yet lie in our biopsychosocial understanding of pain, but our ability to find and implement it depends not on our knowledge but on our systems. Fixing our systems may be a harder pill to swallow.
Jamie Moffa is a PhD candidate at Washington University, USA. You can follow them on Twitter/X – @thatbrass.